Radiation Treatment
What is Radiation?
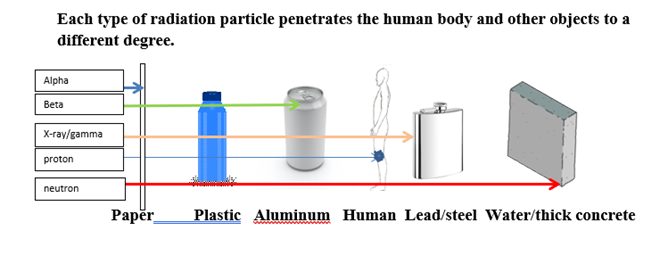
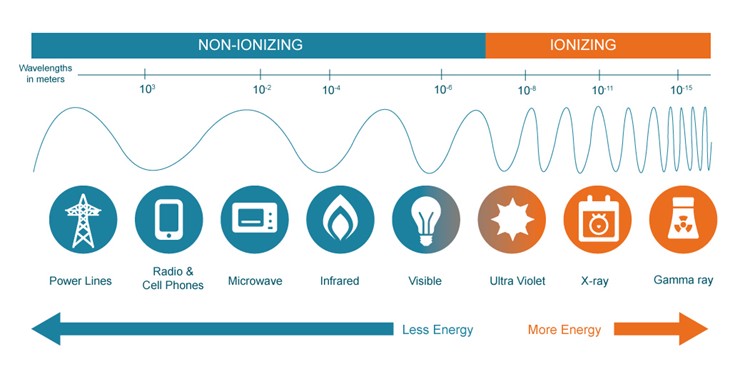
Radiation is an invisible form of energy that travels in waves and at the speed of light. Waves have different energy levels and pass through human tissue to varying depths. For example, sunlight’s ultraviolet radiation can pass into the skin to a depth of around 3 cm (just over 1 inch). Types of radiation differ by wavelength with shorter wavelengths having more energy. Radiation used to control tumours in humans is called ionizing radiation, which has more energy for deeper penetration into the body.
When a pituitary tumour is growing or if surgical and medical treatments fail to control excess hormone production, radiation or radiotherapy is often recommended. A radiation oncologist designs, delivers, and monitors person specific radiation therapy.
How is Radiation delivered?
How is radiation delivered?
Radiation for pituitary tumors is delivered by external beam radiation i.e., the radiation is applied from outside the body and directed at the tumor. The machine used is called a Linear Accelerator.

How does Radiation work?
How does radiation work?
Higher energy ionizing radiation is used. This energy damages the genetic instructions (DNA) for tumor cell multiplication by ‘picking up’ electrons and removing them from the atoms and molecules of tumor tissue. Each time the tumor cell multiplies it has more damage until it can no longer replicate and dies. Although some cells may die immediately, others will die over many years. Normal cells affected by radiation have a better ability to repair themselves than do tumour cells.
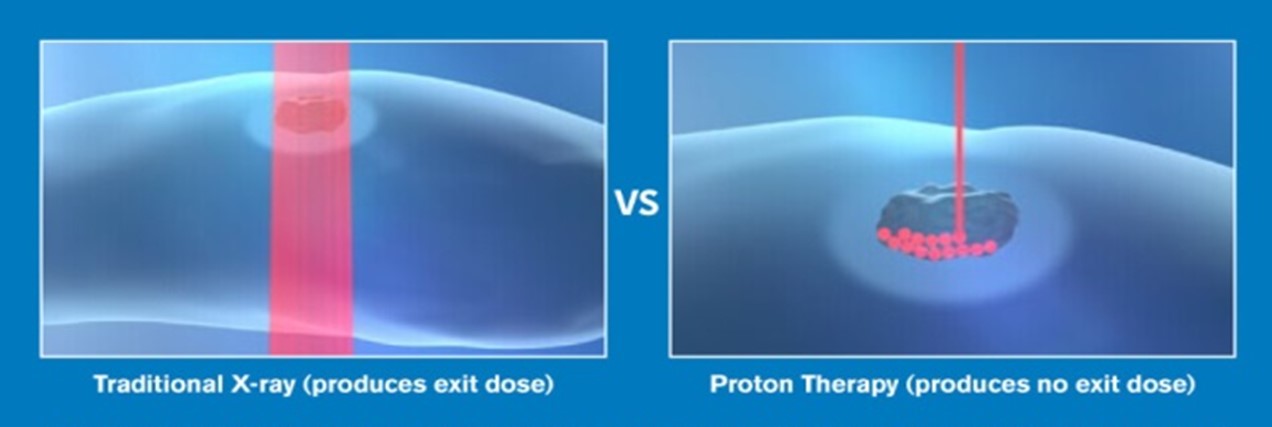
The objective of radiation therapy is to target tumor cells but spare as much damage as possible of the surrounding normal pituitary cells. Ionizing stereotactic forms of radiation (stereotactic radiosurgery [SRS]) are used to target pituitary tumours. This may use proton beams or Intensity Modulated radiotherapy (IMRT) to more precisely focus or ‘conform’ the radiation beam to the 3D shape of the tumor and concentrating damaging energy within the tumour. As the energy passes through the tumour (exit dose), the energy is lowered, sparing damage to normal tissue.
Radiation doses are delivered in a measurement known as Gray (Gy). This is a measure of the amount of radiation absorbed by the patient’s tissue. 1 Gy=1 Joule of radiation absorbed/kg or organ weight (also = 100 rads, which is an old term). The specific dose needed is calculated based on factors such as tumor size, shape, and location.
Stereotactic radiation may be given in multiple small fractions (fractionated) over several weeks (5-6) or in fewer larger doses as Gamma knife or CyberKnife radiosurgery. The Gamma Knife delivers multiple beams at the same time, whereas the CyberKnife System delivers a single, high-energy photon beam to the tumour.
The type and dose of radiation that is appropriate is determined by a radiation oncologist.
Planning CT and MRI
Planning involves obtaining both a computed tomography (CT) and MRI imaging for viewing the tumor in 3D (3 dimensions). From these images the radiation oncologist calculates the dose and direction of radiation beams needed to target the tumour while minimizing damage to the surrounding pituitary.
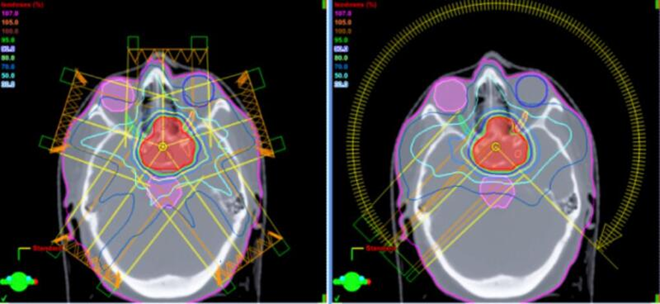
Example of the angle of radiation beams delivered during IMRT treatments to the 3D tumour target (red).
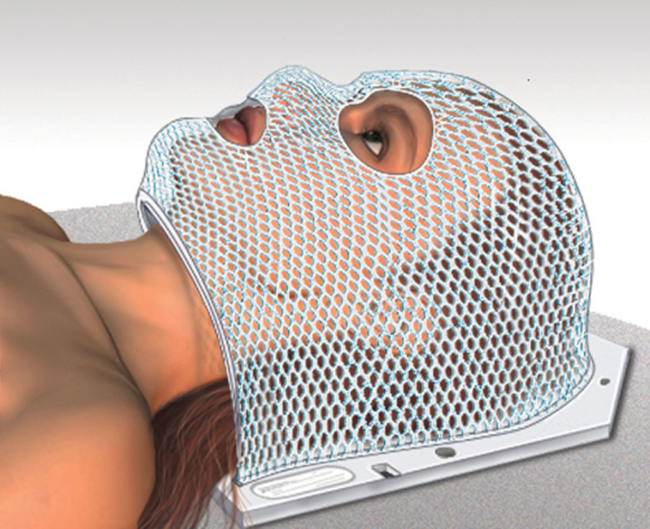
A special lightweight mask is made so that the patient can be positioned exactly and not move for each subsequent treatment. Each treatment usually takes about 30 minutes.
Possible side effects of Radiation
Possible side effects of Radiation
Side effects may be different because of type, location and size of tumor, the total Gy, type of radiation, patient age and sex.
Side effects which may occur are:
– Fatigue is the most common.
– Some skin irritation and changes can occur.
– Nausea and or vomiting.
– Headache.
– Dizziness.
– Hair loss.
– Vision changes are rare, planning is important to avoid damage to the optic nerve structure.
– Problems with memory or thinking.
– Pituitary hormone deficiency may develop over time.
Most Side effects are mild but should be reported to your medical team.
Follow-up after Radiation
Follow up after Radiation
Follow up usually is scheduled with multiple teams, including radiation oncology, endocrinology, neurosurgery.
Every 6 months follow up until stable then every 1-5 years. This includes:
- Magnetic resonance imaging to determine if tumor is stable.
- Testing for pituitary deficiencies, particularly for adrenal insufficiency.
These may appear some time after radiation treatment. - Vision/ ophthalmology exam.
If hormonal excess is present at the time of radiation therapy, ongoing medical therapy is given and reassessed at regular intervals. Control of hormonal excess may take 2 years or longer after radiation treatment.
Life-long follow up is recommended.
Abbreviations
Abbreviations
3D 3 dimensional
CT computerized tomography scan / computerized axial tomography (CAT)
DNA deoxyribonucleic acid (genetic material)
Gy Gray (radiation dose)
IMRT intensity modulated therapy
MRI magnetic resonance imaging
SRS stereotactic radiosurgery
References
References
Kosmin M, Fersht N. Radiotherapy for Pituitary Tumors. [Updated 2020 Nov 6]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
Lian X, Shen J, Gu Z, Yan J, Sun S, Hou X, You H, Xing B, Zhu H, Shen J, Zhang F. Intensity-modulated Radiotherapy for Pituitary Somatotroph Adenomas. J Clin Endocrinol Metab. 2020 Dec 1;105(12):dgaa651. doi: 10.1210/clinem/dgaa651. PMID: 32930785.
Chanson, P., Dormoy, A., & Dekkers, O. M. (2019). Use of radiotherapy after pituitary surgery for non-functioning pituitary adenomas, European Journal of Endocrinology, 181(1), D1-D13. Retrieved Nov 28, 2022, from https://eje.bioscientifica.com/view/journals/eje/181/1/EJE-19-0058.xml
Ramos-Prudencio R, Pérez-Álvarez SI, Flores-Balcazar CH, et al. Radiotherapy for the treatment of pituitary adenomas: A dosimetric comparison of three planning techniques. Rep Pract Oncol Radiother. 2020;25(4):586-593. doi:10.1016/j.rpor.2020.04.020
Author:
Chris Yedinak DNP,FNP.
Associate Professor
Oregon Health & Sciences University Portland. OR. USA
Updated: November 2022
