Hypothyroidism
What is Hypothyroidism?
What is hypothyroidism?
Hypothyroidism means there is insufficient thyroid hormone in the body to support metabolic needs.
Hypothyroidism happens when the thyroid gland fails to produce and circulate enough thyroid hormone in the blood to act on tissues throughout the body. Causes include Primary failure of the thyroid gland itself to produce thyroid hormone or lack of stimulation secondary to a malfunction of the pituitary gland. This is known as central hypothyroidism.
Production Hypothyroidism Hormone
How is thyroid hormone produced?
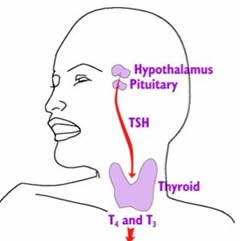
The story of thyroid hormone production begins in the hypothalamus which produces Thyroid Releasing hormone (TRH).
TRH acts on the front or anterior lobes of the pituitary, instructing specialized cells to make thyrotropin also known as thyroid stimulating hormone (TSH).
TSH is the master control hormone that acts on the thyroid gland to manage the production of the active hormones thyroxine (T4) and triiodothyronine (T3).
How is Thyroid Hormone production controlled?
How is thyroid hormone production controlled?
In the follicular cells of the thyroid, a substance called thyroid peroxidase reacts with iodine to form T4 (Thyoxine) and T3(triiodothyronine). Iodine is found in the soil, seawater and some foods, but may not be adequate in some places. In some countries, iodine needs to be added to foods such as salt. T4 & T3 are stored in the thyroid as a molecule called thyroglobulin until needed. T4 and T3 work together to control the metabolic rate of the body or generate energy, heat for muscle and brain function, regulate heart rate, and maintain bones. However, T3 is the most active thyroid hormone in body cells.
When body tissue levels are low, thyroglobulin is broken down into T4 (and some T3) and secreted from the follicular cells into the blood. However, T4 needs to be converted to T3 in peripheral tissues such as in the liver and kidneys and brain and some fat tissue. T3 then circulates in the blood, attaches to receptors in a lock and key fashion and is transported into the target cell nucleus where it performs its function.
After available T4 and T3 have been used, low levels of both signal the cycle to restart, the hypothalamus and the pituitary to release more TRH and TSH and in turn, the follicular cells of the thyroid to make more T4 & T3. This completes a feedback loop.
When a tumor damages the hypothalamus and/or the pituitary, the production of TRH or TSH may be disrupted, causing low thyroid levels. This is known as central or secondary hypothyroidism.
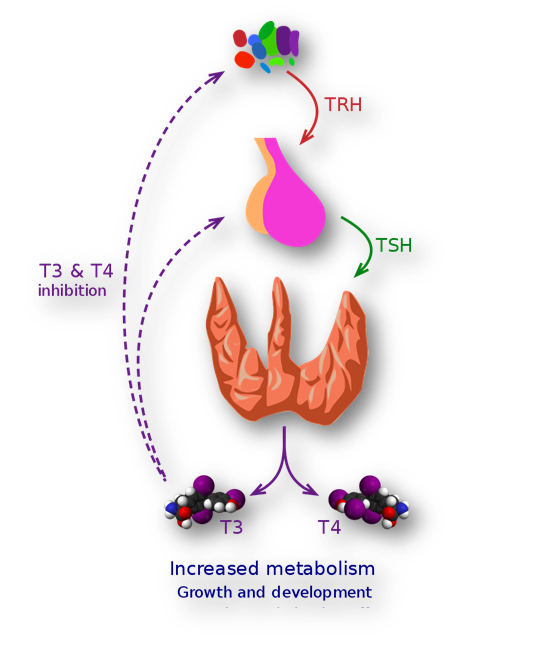
Image: Feedback mechanism in the control of thyroid hormone production.
Symptoms of Hypothyroidism
Symptoms of Hypothyroidism
Symptoms are:
Fatigue and lethargy;
Cold intolerance;
Reduced Appetite;
Constipation:
Dry skin:
Poor memory;
Slow thinking;
Poor concentration;
Anxiety;
Depression;
Irritability;
Stiff muscles cramping and numbness;
Menstrual changes;
Infertility;
Poor sleep.
Signs are:
Puffy face;
Loss of eyebrows;
Hair loss;
Swelling of the tongue;
Slow speech;
A goitre/lump at the front of the neck;
Slow movement;
Low body temperature;
Weight gain;
Low irregular heart rate.
.
How is Hypothyroidism tested?
How is hypothyroidism tested?
To test for central hypothyroidism, a blood sample is drawn to measure the amount of TSH and Free T4 in the blood. Free T4 is the T4 that is available in the blood to attach to receptors. Rarely it is necessary to measure the amount of T3 if Free T4 is adequate.
A number of factors may make testing TSH independently unreliable as an indicator of central hypothyroidism, particularly after a tumour or surgery affecting the pituitary with potential damage to thyrotropes. If Free T4 levels are low normal and TSH is normal, central hypothyroidism should be considered.
Treatment of Hypothyroidism
How is hypothyroidism treated?
N.B. In patients with pituitary disorders and central hypothyroidism, it is vital that adrenal function be tested and determined to be normal prior to starting thyroid replacement. If adrenal insufficiency is present, thyroid supplementation can increase the metabolic need for cortisol and precipitate an adrenal crisis.
Most commonly, replacement with levothyroxine (LT4) is prescribed. For better absorption in the intestines, this tablet is taken first thing in the morning 30-60 minutes prior to eating. Low T3 has been considered rare until recent questions have been raised about sufficiency of T3 in the context of central hypothyroidism treated with T4 only. In these cases, a combination of T4 and T3 may be recommended. This is an ongoing debate.
A Blood test is recommended 6-8 weeks after started levothyroxine and 4-8 weeks after each dose adjustment. The most common goal is to keep the Free T4 level in about the middle of the normal range.
When monitoring thyroid levels, it is also important to consider the circadian pattern of Thyroid production. Taking high doses of biotin may also affect the accuracy of testing and should be discontinued about 7 days prior to testing per some clinicians.
If levels become too high, symptoms of hyperthyroidism may occur such as irregular, fast heart rate, bounding pulse, heat intolerance & sweating, weight loss, diarrhea and more.
Abbreviations
Abbreviations
TRH thyroid releasing hormone
TSH thyroid stimulating hormone
FT4 free thyroxine
T3 thyronine
References
References
Mahadevan S, Sadacharan D, Kannan S, Suryanarayanan A. Does Time of Sampling or Food Intake Alter Thyroid Function Test?. Indian J Endocrinol Metab. 2017;21(3):369-372. doi:10.4103/ijem.IJEM_15_17
Beck-Peccoz P, Rodari G, Giavoli C, Lania A. Central hypothyroidism – a neglected thyroid disorder. Nat Rev Endocrinol. 2017 Oct;13(10):588-598. doi: 10.1038/nrendo.2017.47. Epub 2017 May 26. PMID: 28549061.
Idrees T, Palmer S, Maciel RMB, Bianco AC. Liothyronine and Desiccated Thyroid Extract in the Treatment of Hypothyroidism. Thyroid. 2020 Oct;30(10):1399-1413. doi: 10.1089/thy.2020.0153. Epub 2020 May 12. PMID: 32279609; PMCID: PMC7640752.
Author:
Chris Yedinak DNP,FNP.
Associate Professor
Oregon Health & Sciences University Portland. OR. USA
Updated: November 2022
