Craniopharyngioma
What is a Craniopharyngioma?
What is a craniopharyngioma
A craniopharyngioma is a non-cancerous tumour, likely formed in utero, that grows inside or on top of the pituitary. These tumors can grow to affect and adhere to structures such as the hypothalamus, the optic nerves, and the cavernous sinus.
They most often are found in childhood or after the age of 50 and equally for men and women. They are slow growing tumors that can affect the pituitary hormone production and the function of nearby structures. Craniopharyngiomas do not secrete any hormones.
How are Craniopharyngioma’s found?
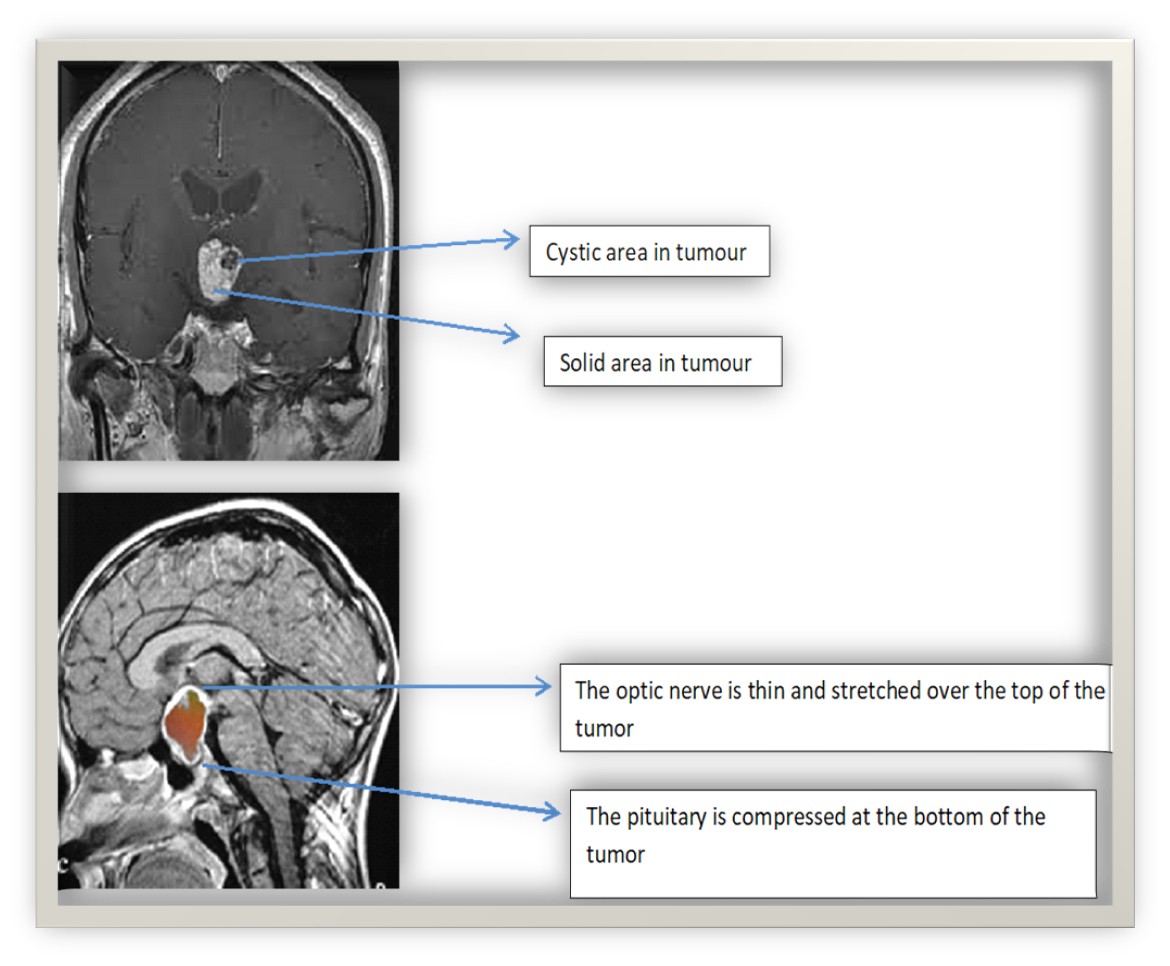
Craniopharyngiomas are usually large when discovered on magnetic resonance imaging (MRI). They are identified by having both cystic and solid parts. They are often found when they grow up and out of the pituitary and around the optic nerve or the optic chiasm where the nerves from the eyes cross and enter the brain affecting vision. They may also grow between the pituitary and the hypothalamus, impacting the hypothalamus causing symptoms such as weight gain. If they grow into the area beside the pituitary, the cavernous sinus, they may affect the movement and ability of the eyes to focus.
Because of their large size, craniopharyngiomas can put pressure on the pituitary stalk and interrupt the signal to decrease the production of prolactin so prolactin level increases. Other pituitary hormone production may also be decreased because of compression of other cells as the tumour grows.
They can interrupt the nerve signals to the posterior (back) pituitary to release antidiuretic hormone causing frequent urination and arginine vasopressin deficiency (AVP-D) previously known as diabetes insipidus.
Symptoms
What are the symptoms associated with a craniopharyngioma?
The following symptoms could occur with craniopharyngioma:
Headaches are common at all ages.
Peripheral field vision loss, eye movement weakness/double vision as the tumour grows and affects the optic nerves.
Excessive thirst and urination (AVP-D/ diabetes insipidus) with the involvement of the posterior (back) of the pituitary.
Nausea & low blood pressure if there is adrenal insufficiency or vomiting with increased intracranial pressure.
Fatigue and increased sleepiness.
Sexual dysfunction.
Personality changes and confusion.
Stunted growth or delayed puberty in children and Growth hormone deficiency in adults.
Constant hunger and weight gain if hypothalamus is involved.
Hot/cold intolerance may be due to damage to the hypothalamus and/or thyroid stimulating hormone dysfunction from damage to cells in the pituitary.
Menstrual irregularities and lack of menstrual cycle associated with elevated prolactin due to pressure on the pituitary stalk (stalk effect) from a growing tumour.
Assessments, Diagnosis and Testing
Assessments, Diagnosis and Testing
Often the patient notices a change in vision first. Visual assessment with an ophthalmologist and visual field exam can determine if there is pressure on the optic nerve.
MRI confirms the presence of a tumor. These tumors have a characteristic appearance on Magnetic Resonance Imaging (MRI) with both cystic areas and solid areas.
Pituitary function testing to evaluate all hormone levels is recommended because of hormone deficiencies that occur because the cells are compressed and unable to function properly.
Blood tests for pituitary function include:
- A cortrosyn stimulation test for adrenal insufficiency
2.Thyroid function testing with both a TSH (thyroid stimulating hormone) and FT4 (free thyroxine) level
- Prolactin level to evaluate for a prolactin producing tumor versus pressure on the pituitary stalk.
- IGF-1 (insulin growth factor-1) as a preliminary evaluation for growth hormone deficiency.
- Gonadal function tests, LH (luteinizing hormone), FSH (follicle stimulating hormone) and testosterone levels in males
- Electrolytes, urine, and serum osmolality will be evaluated for symptoms of arginine vasopressin deficiency (AVP-D/ diabetes insipidus) if frequent urination and thirst.
Treatment
Treatment
There is currently no medical therapy to treat craniopharyngioma.
Surgery to remove the tumor is recommended with a neurosurgical team experienced in the removal of pituitary tumors. Pathology performed on the tumour specimen removed will confirm a diagnosis.
Glucocorticoids such as hydrocortisone may be administered post operatively until testing can confirm no evidence of ‘adrenal insufficiency’. This can occur if ACTH (adrenocorticotrophic hormone) is not secreted normally post operatively.
Post operative pituitary hormone function testing is recommended, including adrenal function to evaluate the need for hydrocortisone. Replacement therapy for hormone deficiency may be needed.
Monitoring symptoms of increased thirst and frequent urination or for the development of AVP-D (diabetes insipidus) and for SIADH (syndrome of inappropriate antidiuretic hormone) with blood electrolyte levels while in hospital and after discharge is important.
In the event of weight gain related to hypothalamic damage, other treatments may be needed from nutritionists and weight management specialists.
Craniopharyngiomas can grow or grow back slowly over time. The chance of recurrence may be as high as 50%. After the post operative period, an MRI at least every 5 years and regular follow up with an endocrinology team and ophthalmologist is recommended.
Repeat surgery and radiation therapy are treatment options should the craniopharyngioma grow back.
Abbreviations
Abbreviations
ACTH Adrenocorticotrophic Hormone
MRI Magnetic Resonance Imaging
AVP-D Arginine Vasopressin Deficiency
IGF-1 Insulin Growth Factor-1
LH Luteinizing Hormone
FSH Follicle Stimulating Hormone
References
References
Ortiz Torres M, Shafiq I, Mesfin FB. Craniopharyngioma. [Updated 2022 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
Müller HL, Merchant TE, Warmuth-Metz M, Martinez-Barbera JP, Puget S. Craniopharyngioma. Nat Rev Dis Primers. 2019 Nov 7;5(1):75. doi: 10.1038/s41572-019-0125-9. PMID: 31699993.
Yedinak, CG. Sella and Suprasella Brain Tumors and Infiltrative Disorders Affecting the HPA-Axis. In S.Llhana, C.Follin, C.Yedinak & A.Grossman (Eds). Advanced Practice in Nursing Endocrinology. Springer Publishing Company 2019:255-275
Honegger J, Tatagiba M. Craniopharyngioma surgery. Pituitary. 2008;11(4):361-73. doi: 10.1007/s11102-008-0137-z. PMID: 18636330.
Amayiri N, Spitaels A, Zaghloul M, Figaji A, Cavalheiro S, Muller HL, Elhassan M, Parkes J, Mushtaq N, Beltagy ME, Yousef YA, Esiashvili N, Sullivan M, da Costa MD, Dastoli P, Mubarak F, Bartels U, Chamdine O, Davidson A, Musharbash A, Alcasabas P, Bouffet E, Bailey S. SIOP PODC-adapted treatment guidelines for craniopharyngioma in low- and middle-income settings. Pediatr Blood Cancer. 2020 Aug 13:e28493. doi: 10.1002/pbc.28493. Epub ahead of print. PMID: 32790146.
Author:
Chris Yedinak DNP, FNP
Associate Professor
Oregon Health & Sciences University Portland. OR. USA
Updated November 2022
