Pituitary Surgery
Why Surgery?
Why Surgery?
Surgery may be recommended to remove a tumor that is in, or affecting, the pituitary gland. Pituitary tumors are present in 1 in 4 people, most of whom are unaware and have no symptoms. Less than 0.1% of pituitary tumors are cancerous or malignant and less than 10% of all pituitary tumors require surgery.
Surgery may be recommended for one of several reasons:
- There is a large tumor known as a macroadenoma, usually larger than 1cm.
- tumor that has shown growth on follow up brain imaging or magnetic resonance imaging (MRI).
- Tumor that is pushing on the nerves for the eyes or the ‘optic chiasm’, and causing vision loss, particularly peripheral vision loss in one or both eyes.
- Tumor that is making too much of a one type of pituitary hormone or hypersecretory.
- Tumor that cannot be controlled with medication.
- To examine the cells of the tumor to make a diagnosis (i.e., pathology is needed).
What to know about Surgery?
What to know about Surgery?
Recommendations Prior to Surgery:
- A specialized eye exam or visual field from an eye doctor or neuro-ophthalmologist.
- Magnetic resonance imaging (MRI) of the brain with extra views of the pituitary.
- Imaging of the brain blood vessels, called an MRA, to determine your specific major vessel locations.
- Endocrine testing to evaluate the pre-operative amount (too much or too little) of each pituitary hormone, including: prolactin, growth hormone & IGF-1, cortisol and adrenocorticotropic hormone (ACTH), thyroid stimulating hormone (TSH), free thyroxine (Free T4), luteinizing hormone (LH), follicle stimulating hormone (FSH) and electrolytes such as sodium and potassium. Further specialized testing such as a dynamic test for adrenal function or medicines, may be needed prior to surgery.
- Explanation of surgical risks and benefits is usually given by the surgical team and the endocrine team and include further pituitary hormone damage, vision damage, bleeding, infection, temporary loss of taste and smell, arginine vasopressin deficiency (AVP-D/ diabetes insipidus), syndrome of inappropriate antidiuretic hormone (SIADH).
What happens during the Surgical Procedure?
What happens during the surgical procedure?
FOUR different medical and surgical teams are involved in a pituitary surgery
- Anesthesia team:
- Assess patients’ history and airway prior to giving sedation and anesthesia
- Manage fluid administration during the operation: An intravenous catheter is placed in veins to give fluids, medicines and to take blood samples
- Manage patient breathing by placing a breathing tube, usually through the mouth, that attaches to a breathing machine while the patient is asleep.
- The anesthesia team monitors the patient’s vital signs, heart rate, blood pressure, blood electrolyte levels and more throughout the procedure and during the recovery period.
- The Ear, Nose and Throat (ENT) team:
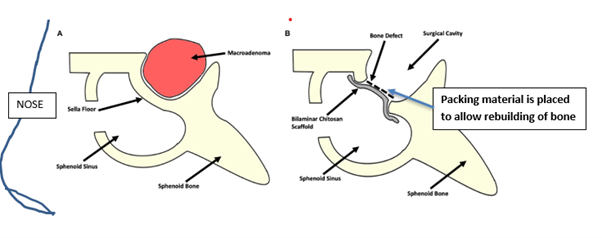
- Once the patient is under anesthesia, the ENT surgeon makes an incision inside one side of the nose. They remove tissue and bone to open a small hole into the pituitary sella (the protected bone around the pituitary).
- At the end of the surgery ENT surgeons ‘sew up’ or close any wounds in the nose. They may place surgical packing in the nose that may need to be removed from several days to 1-2 weeks after surgery.
- Neurosurgery team:
- Place either a special endoscope or microscope tube through the side of nose to see and remove the tumour.An endoscope is a thin tube with a high-powered camera and light at the end through which small instruments can be advanced. The camera view is also projected onto a large TV screen for viewing by the surgical team.If a microscope is used, it’s attached to an endoscope. the surgeon looks through the microscope to view the surgical area.
- Use special instruments and suction tube through the endoscope to remove tumour, tissue samples and blood. The tumor is usually removed in pieces small enough to pass through the suction device. As much of the tumor as possible is preserved for the pathologist to examine usually after the surgery.
- Sometimes an imaging or MRI technique is used to help the surgeon navigate more exactly to the location of the tumor.
- When all the visible tumour is removed, the area is assessed for any leakage of cerebrospinal fluid. The hole in the bone underneath the pituitary is then filled with either a surgical packing material or a small amount of the patients’ own fat tissue that is taken from just under the skin, most often of the abdomen. If a cerebrospinal fluid (CSF) leak is found, the anesthesia team will place a small catheter into the spinal canal in the lower back to keep the pressure in the spinal column low and allow the leak to heal. This is usually removed around 72 hours after surgery.
- After surgery, patients are observed in hospital for 1-3 days for: Cerebrospinal fluid leak, headaches, need for pain medication, vision changes, fluid balance ( liquid consumed and the volume of urine each day). Blood is tested for sodium levels frequently.
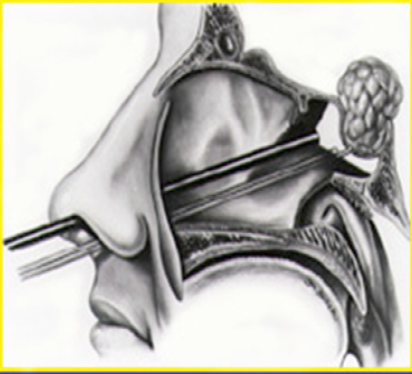
The Endoscope is placed in the nostril and the bony sella floor is removed.
- Endocrine team
Patients are monitored for symptoms of several pituitary hormone deficiencies.- Adrenal insufficiency (AI) or failure of pituitary adrenocorticotropic hormone (ACTH) to stimulate the adrenal glands.
Symptoms of AI include headaches, nausea, dizziness, and vomiting. It’s notable that headaches are not uncommon after this surgery. Glucocorticoid replacement medications, such as hydrocortisone, will be given if needed or in some centers until the ability of the adrenal glands to produce cortisol can be tested around 12-14 days after surgery. - Patients are monitored for arginine vasopressin deficiency /diabetes insipidus. This includes:
a. Regular blood draws for sodium levels (high sodium);
b. Blood and urine testing for osmolality (concentration);
c. The total amount of fluid taken in and the volume of urine out;
d. Patient’s thirst and how frequently they are urinating during the day and at night.Treatment with medication such as vasopressin or desmopressin may be given if needed.
- After discharge blood electrolytes will be monitored for the development of Syndrome of Inappropriate Anti-diuretic Hormone (SIADH) or low sodium. Patients and family are instructed to monitor for changes in mental state such as confusion and notify the endocrine team.
- If hormone excess is known before surgery blood levels of cortisol, ACTH, growth hormone (IGF-1) levels or prolactin levels may also be checked immediately post operatively.
- Adrenal insufficiency (AI) or failure of pituitary adrenocorticotropic hormone (ACTH) to stimulate the adrenal glands.
Expected Symptoms After Surgery
Expected symptoms after surgery
The following symptoms may occur:
– Headaches: Usually decreasing over 1-2 weeks after surgery.
– Nasal tenderness: particularly on the surgical side.
– Congestion: dry mouth if nose is blocked.
Sterile saline nasal spray may be recommended by your team to use several times daily.
– Blood-tinged drainage: Saline flushes may be helpful as per your teams’ instructions
Symptoms to report URGENTLY to your Surgical or Endocrine team
Symptoms to report URGENTLY to your Surgical or Endocrine team
– Headaches that are getting worse.
– Confusion
– Headaches plus dizziness and nausea and/or vomiting.
– Fainting
– Sticky clear fluid draining from nose.
– Yellow and green drainage from your nose.
– Fever
– Stiff neck
– Severe thirst and frequent urination such as every hour.
– Blind spots in your vision that are getting worse.
– Severe nosebleed that is difficult to stop.
Post-Operative Follow-Up
Post-operative follow-up
Follow-up will be scheduled with each team and may vary according to centre. Endocrine follow up is usually more frequent immediately post operatively from every 2-6 weeks.
Post op endocrine testing will be conducted to evaluate any changes to pituitary function. These may include dynamic testing of adrenal function, pituitary hormone levels and other specialized testing according to diagnosis.
MRI will usually be evaluated at 3 months post operatively and every 6-12 months or more if stable.
An ophthalmology visual field exam may be recommended to establish a post operative baseline for future measurements.
Abbreviations
Abbreviations
AI adrenal insufficiency
ACTH adrenocorticotropic hormone
AVP-D arginine vasopressin deficiency /diabetes insipidus
CSF cerebrospinal fluid
FT4 free thyroxine
IGF-1 insulin growth factor-1
MRI magnetic resonance imaging
MRA magnetic resonance angiography
SIADH syndrome of inappropriate antidiuretic hormone
TSH thyroid stimulating hormone
References
References
Deopujari CE, Shaikh ST. Evolution of Pituitary Surgery. Neurol India. 2020 May-Jun;68(Supplement):S33-S38. doi: 10.4103/0028-3886.287673. PMID: 32611890.
Majovsky M, Astl J, Kovar D, Masopust V, Benes V, Netuka D. Olfactory function in patients after transsphenoidal surgery for pituitary adenomas-a short review. Neurosurg Rev. 2019 Jun;42(2):395-401. doi: 10.1007/s10143-018-1034-1. Epub 2018 Oct 1. PMID: 30276575.
Miller BA, Ioachimescu AG, Oyesiku NM. Contemporary indications for transsphenoidal pituitary surgery. World Neurosurg. 2014 Dec;82(6 Suppl):S147-51. doi: 10.1016/j.wneu.2014.07.037. PMID: 25496626.
Joshi SM, Cudlip S. Transsphenoidal surgery. Pituitary. 2008;11(4):353-60. doi: 10.1007/s11102-008-0094-6. PMID: 18369724.
Chin SO. Epidemiology of Functioning Pituitary Adenomas. Endocrinol Metab (Seoul). 2020;35(2):237-242. doi:10.3803/EnM.2020.35.2.237
Author:
Chris Yedinak DNP,FNP.
Associate Professor
Oregon Health & Sciences University Portland. OR, USA
Updated: November 2022
