Non-Functional Pituitary Adenoma (NFA)
What is a non-functional pituitary adenoma?
What is a non-functional pituitary adenoma?
A non-functional adenoma (NFA) or tumor in the pituitary is an abnormal collection of cells that do not produce excessive hormone. NFAs represent about 30% of all pituitary adenomas
NFAs are benign and non-cancerous. They are often found ‘incidentally’ on magnetic resonance imaging (MRI) done for other reasons. Pituitary tumors are thought to be found in 1 in 4 people but only 1 out of 1,000 may need any treatment.
NFAs are usually small < 1cm (10mm) and called microadenomas. They are often not associated with symptoms. These are “watch and wait tumors”, and the patient will be followed for changes in symptoms, vision, or tumor growth.
An NFA can grow and become large enough to cause damage to the pituitary or surrounding structures such as the nerves for the eyes or optic nerves (see images a,b,c d below)
Tumors >1cm are called macroadenomas and may need to be removed surgically if impacting the vision structures (optic nerves or optic chiasm). (see image c)
There is currently no medicine that will shrink an NFA
When is removing of tumor recommended?
When is removing the tumor recommended?
It is recommended to remove the tumor when the following situations or symptoms occur:
1.Headaches – Large tumors that cause severe headaches.
2.If bleeding occurs inside the tumor and causes a sudden onset severe headache. This is known as apoplexy. This is an endocrine emergency requiring surgery and replacement of cortisol immediately.
3. A macroadenoma pushing on the optic nerves causing loss of peripheral vision in one or both eyes. This is called ‘mass effect’. The location of pressure on the optic nerve will affect which eye is affected. In severe cases, peripheral vision in both eyes is lost and only central or ‘tunnel’ vision remains, or all vision is lost. Removal of the tumor will frequently restore vision.
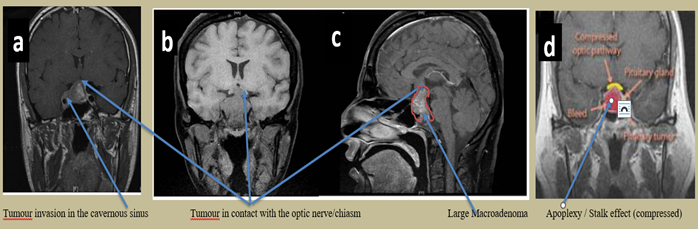
4.If the tumor grows into the cavernous sinus area beside the internal carotid arteries, nerves controlling eye movement can be affected, causing double vision and inability of the eyes to focus. (see image a).
5. If there is a need for a biopsy to determine the exact type of tumor to direct post-operative treatment planning. Pathology can also determine if there is rapid cells multiplication, which may indicate a higher risk of any residual tumor regrowth or recurrence.
Symptoms of a Non-Functioning Pituitary Adenoma (NFA)
Symptoms of a non-functioning pituitary adenoma (NFA)
Often there are no symptoms.
Headache is the most common symptom for both micro and macroadenomas.
Vision changes may occur with progressive peripheral vision loss in one or both eyes. If this continues as the tumor grows, blindness can result. (see images above).
Sometimes prolactin level may be a little high. This happens when there is pressure on the pituitary stalk and the messages to stop prolactin production are not relayed to the prolactin producing cells of the pituitary. (see image c).
Hormonal deficiencies may occur: Low ACTH and adrenal insufficiency, low thyroid levels, low follicle stimulating hormone (FSH) and luteinizing hormone (LH), menstrual irregularities, and low testosterone in males, along with sexual problems (hypogonadism).
Low growth hormone in adults can result in loss of lean body mass and muscle, weight gain, memory loss, poor bone density, social isolation and more.
Types of Non-Functioning Adenomas by Pathology
Types of non-functioning adenomas by pathology
Gonadotroph adenomas are considered non-functional adenomas. However, these may rarely secrete higher levels of luteinizing hormone (LH) and follicle stimulating hormone (FSH). Often these levels are low.
Null cell adenomas do not show any cell type on pathology
Silent adenomas are tumor cells that make adrenocorticotrophic hormone (ACTH), growth hormone, prolactin or thyroid stimulating hormone (TSH), but blood and other tests done prior to surgery show these hormone levels are normal. Silent hormone producing adenomas may be more likely to regrow at a faster rate than other types of adenomas. Testing is also needed after surgery more frequently to monitor for excess hormone production.
The pathologist can also examine the granulation pattern of the cells in a tumor. Those that are sparsely granulated are also known to behave more aggressively and grow faster. These require more regular follow-up.
Rathke’s cleft cysts form from remnants of embryonic development after the roof of the mouth folds upward to form the anterior and posterior lobes of the pituitary. The gap in between these lobes is Rathke’s pouch. If the opening closes a cyst can form. Headache is the most likely symptom, which is often resolved or improved with surgical removal of the cyst.
Meningiomas are tumors that form around the membrane (meninges) that covers the brain. If they grow above the pituitary, they can affect the optic nerve and cause vision loss or deficiencies of pituitary hormones.
Craniopharyngiomas are non-cancerous, benign tumors. Images show some areas of solid tumor and some cysts. These can be very large and are found growing in, and above or out of, the pituitary. They can affect the optic nerves causing vision loss and blindness and deficiencies in pituitary hormones. If the hypothalamus above the pituitary is affected, the patient may have significant weight gain.
Follow-up
Follow-up
– microadenoma may only require monitoring every 1-3 years if all pituitary functions are normal with increasing intervals with ongoing stability.
-Recurrence of NFA may occur in an estimated 1/4 of cases within the first 5-10 years post operatively with a higher likelihood (over 40%) of those with residual tumour postoperatively, particularly with invasion of the cavernous sinus.
-After the surgical removal of a large macroadenoma, monitoring for growth of any residual pituitary adenoma or recurrence with MRI is recommended 3 months after surgery and every 6 months until stable, then every year for first 5 years. Imaging interval may increase over time if stable, but lifelong follow up is recommended.
-Pre and post-operative endocrine testing of all pituitary functions with every 3-6 month follow up until stable then every 6-12 months
-With ophthalmology exams with visual field testing in between MRIs can detect pressure on the optic nerve and the need for more urgent imaging.
-Reoperation is usually recommended if a NFA regrows. Radiation therapy may also be recommended if the adenoma regrows yet again.
-If the adenoma fails to respond to surgery plus radiation, then the chemotherapy agent Temozolomide has been useful in patients with specific tumor characteristics.
Abbreviations
Abbreviations
ACTH adrenocorticotropic hormone
FSH follicle stimulating hormone
LH luteinizing hormone
NFA non-functional adenoma/no hormone secretion
MRI magnetic resonance imaging
References
References
Chanson P, Raverot G, Castinetti F, Cortet-Rudelli C, Galland F, Salenave S; French Endocrinology Society non-functioning pituitary adenoma work-group. Management of clinically non-functioning pituitary adenoma. Ann Endocrinol (Paris). 2015 Jul;76(3):239-47. doi: 10.1016/j.ando.2015.04.002. Epub 2015 Jun 10. PMID: 26072284.
Esposito D, Olsson DS, Ragnarsson O, Buchfelder M, Skoglund T, Johannsson G. Non-functioning pituitary adenomas: indications for pituitary surgery and post-surgical management. Pituitary. 2019 Aug;22(4):422-434. doi: 10.1007/s11102-019-00960-0. PMID: 31011999; PMCID: PMC6647426.
Lyu W, Fei X, Chen C, Tang Y. Nomogram predictive model of post-operative recurrence in non-functioning pituitary adenoma. Gland Surg. 2021 Feb;10(2):807-815. doi: 10.21037/gs-21-47. PMID: 33708562; PMCID: PMC7944052.
Tampourlou M, Ntali G, Ahmed S, Arlt W, Ayuk J, Byrne JV, Chavda S, et al. Outcome of Nonfunctioning Pituitary Adenomas That Regrow After Primary Treatment: A Study From Two Large UK Centers, The Journal of Clinical Endocrinology & Metabolism, Volume 102, Issue 6, 1 June 2017, Pages 1889–1897, https://doi.org/10.1210/jc.2016-4061
Chanson P, Dormoy A, Dekkers OM. Use of radiotherapy after pituitary surgery for non-functioning pituitary adenomas. Eur J Endocrinol. 2019 Jul;181(1):D1-D13. doi: 10.1530/EJE-19-0058. PMID: 31048560.
Author:
Chris Yedinak DNP,FNP.
Associate Professor
Oregon Health & Sciences University Portland. OR. USA
Updated: November 2022
