Diabetes insipidus – Arginine Vasopressin Deficiency (AVP-D) and Syndrome of Inappropriate Antidiuretic Hormone (SIADH)
AVP-D was previously known as Diabetes Insipidus. Diabetes meaning ‘to pass through’, and insipidus ‘lacking’ did not clearly describe the problem of frequent urination owing to a lack of ADH and the inability of the kidneys to reabsorption water. This was frequently confused with Diabetes Mellitus or frequent urination caused by the body’s efforts to rid itself of excess sugar.
What is Antidiuretic Hormone
What is Antidiuretic Hormone (ADH)?
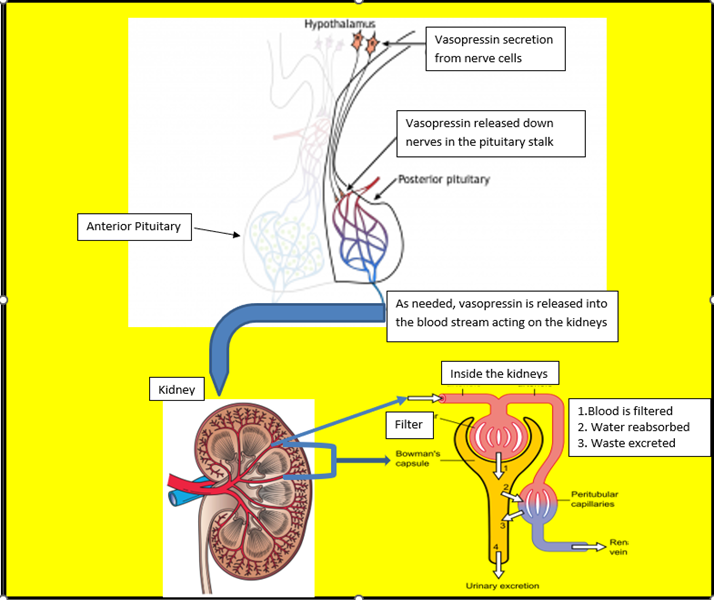
Antidiuretic hormone (ADH) is also known as arginine vasopressin. ADH is a hormone that is made in the hypothalamus and released from nerves down the pituitary stalk and into the posterior pituitary. It is released into the blood stream as needed to maintain a stable amount of water in the body.
Abnormal production or release of ADH causes either ‘too little or too much water’ to be reabsorbed into the blood by the kidneys.
How does ADH work and why
How does ADH work and why?
The total blood volume in humans is about 5 liters with men having a slightly higher volume than women. However, in women blood volume increases about 50% during pregnancy. Maintaining blood volume is critical to supply all cells, tissues and organs with essential energy, nutrients, and substances to fight infection. There are multiple mechanisms to ensure blood volume and subsequent blood pressure is adequately balanced. ADH is a key mechanism.
The body has strategically placed volume and osmolality (concentration) sensors in areas such as the heart and blood vessels of the neck and the hypothalamus. When blood pressure is low, blood volume is lost or the body senses dehydration, signals are sent to several groups of cells in the hypothalamus instructing them to make and secrete ADH. Hypothalamic thirst mechanisms are also activated.
Pain, nausea, low blood sugar levels, narcotic and some other medications can trigger ADH production. In contrast, alcohol stops ADH production and urinary frequency results.
When ADH is produced, it travels down nerve fibers in the pituitary stalk (infundibulum) to the posterior or back lobes of the pituitary also called the pars nervosa. From the posterior pituitary, it is released into a rich network of blood vessels for distribution around the body.
ADH has two actions, one on the kidney and, the other on the muscles around blood vessels. ADH instructs the kidneys to soak up water, keeping the correct amount of water in the blood vessels and bringing the concentration and volume of the blood back to normal. Second, ADH acts on smooth muscles cells in the arteries causing them to constrict, which subsequently increases the blood pressure.
When body sensors register the concentration and volume correction, the hypothalamus is instructed to stop the increased ADH secretion and return to normal baseline levels.
What happens when ADH secretion is abnormally low?
What happens when ADH secretion is abnormally Low?
Arginine Vasopressin Deficiency (AVP-D) is antidiuretic hormone deficiency or low levels or ADH. When ADH is low or inadequately produced, the kidneys do not receive signals to soak up water. This can result in frequent urination, dehydration and low blood volume.
Symptoms
The patient experiences extreme thirst that constant drinking does not quench urination as frequent as several times an hour or more, day and night. Dry mouth, lips and skin, weakness, fatigue, loss of appetite and cramping may also occur. If fluid intake does not keep up with fluid out by urination, dehydration, or high sodium levels result. Blood pressure may increase to compensate for low blood volume. Urine is usually very pale yellow or colorless.
AVP-D may occur after a head injury, surgery for a pituitary tumor, or damage to the pituitary stalk. Some infections and immune diseases that affect the pituitary and/or the hypothalamus may also result in AVP-D. Rarely, the kidney’s do not respond to ADH causing a ‘nephrogenic form’ of AVP-D.
Diagnosis
Assessment of blood sodium and electrolyte levels, blood, and urine osmolality (concentration) are needed for diagnosis and guided by patient symptoms.
Treatment
Treatment is to administer vasopressin or desmopressin, usually as a nasal spray, by mouth in a tablet form or as an oral melt (under the tongue). Post pituitary surgery, AVP-D most frequently resolves from 1-12 weeks post operatively and may be controlled with one or two doses of medication. Patients are recommended to monitor urinary frequency at home, particularly during sleep and discuss discontinuing desmopressin with their endocrine team when symptoms resolve.
What happens when ADH secretion is too high
What happens when ADH secretion is too high?
Syndrome of Inappropriate Antidiuretic hormone (SIADH) occurs when excess ADH is secreted unnecessarily and in excess amounts causing too much water to be reabsorbed by the kidneys. The level of sodium in the blood becomes diluted and low. In SIADH the kidneys can usually still excrete salt and along with salt water is excreted. This acts to decrease the volume in the blood and avoid some swelling. However, this can also make the sodium level in the blood lower.
SIADH may follow pituitary surgery, even after initial symptoms of AVP-D. Other causes can be related to cancer which can produce ADH, stroke, hemorrhage, infection, trauma and some medications.
Symptoms
Symptoms may include decreased thirst, decreased urination with dark yellow urine, headache, confusion, seizures, and death from respiratory arrest if sodium is very low and not treated quickly.
Diagnosis
SIADH may occur up to 2 weeks post operatively. Blood is usually drawn several days after hospital discharge to monitor sodium levels, particularly after larger tumors have been removed. Patients and families are instructed to monitor for symptoms of confusion, nausea, fatigue, and excessive sleepiness and contact their endocrine team immediately.
Treatment
Water needs to be removed from the body, so drinking water and fluid not containing salt is severely restricted. Water may not be recommended at all and only salt containing drinks such as salty broth may be given. Salt (sodium Chloride) may also be given as a capsule or table by mouth, in food, or in the form of intravenous fluid if sodium in the blood is very low. In urgent circumstances, specialty intravenous medications will be administered to increase sodium. Sodium is usually corrected slowly over 24-48 hours to avoid causing neurologic damage.
Abbreviations
Abbreviations
AVP Arginine Vasopressin
AVP-D Arginine Vasopressin Deficiency
ADH Antidiuretic Hormone
DI Diabetes Insipidus h(NB. This diagnosis is now AVP-D)
SIADH Syndrome of Inappropriate Antidiuretic Hormone
References
References
Sharma R, Sharma S. Physiology, Blood Volume. 2022 Apr 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 30252333.
Almalki MH, Ahmad MM, Brema I, et al. Management of Diabetes Insipidus following Surgery for Pituitary and Suprasellar Tumours. Sultan Qaboos Univ Med J. 2021;21(3):354-364. doi:10.18295/squmj.4.2021.010
The Working Group for Renaming Diabetes Insipidus, Arima, H., Cheetham, T., Christ-Crain, M., Cooper, D., Gurnell, M., Drummond, J. B., Levy, M., McCormack, A. I., Verbalis, J., Newell-Price, J., & Wass, J. A. H. (2022). Changing the name of diabetes insipidus: a position statement of The Working Group for Renaming Diabetes Insipidus, Endocrine Connections, 11(11), e220378. Retrieved Nov 24, 2022, from https://ec.bioscientifica.com/view/journals/ec/11/11/EC-22-0378.xml
Author:
Chris Yedinak DNP, FNP
Associate Professor
Oregon Health & Sciences University, Portland. OR. USA
Updated: November 2022
